M.E. is a neurological disease(1) and stands for Myalgic Encephalomyelitis.
My = muscle
Algic = pain
Encephalo = brain
Mye = spinal cord
Itis = inflammation
It is an injury to the Central Nervous System[1], usually triggered by an infectious disease process, e.g. a virus, or by chemicals over stimulating the immune system.[2] It is a multi-system disease, affecting not only the neurological system but also the immune, musculoskeletal, endocrine (hormonal) and cardiovascular systems.[3]
Prognosis is variable depending on how much and which part of the brain has been damaged.[4] Complete pre-illness recovery is rare but possible (around 6% of cases.) [5] Some improvement, even marked improvement (different from full remission) is more likely than complete recovery, although relapses can occur several years after remission.[6] Most cases stabilise at varying degrees of disability. Around 30% of cases are progressive and degenerative [7] and degeneration of end organs may result in death [8]. (One quote of early death rate in M.E. is 10%. This figure includes suicides.[9] Early death from cardiac pathology is put at 2%.[10] Pancreatic failure can also contribute to early death.[11])
Symptoms can be multiple and vary from person to person but common symptoms include post-exertional malaise, cognitive problems (such as short-term memory loss and concentration difficulties), muscle and nerve pain, muscle weakness, noise and light sensitivity, sleep and temperature disturbance, orthostatic intolerance (inability to sustain upright activity e.g. standing, sitting or walking) and sensitivity to food, alcohol, chemicals and medicines. There may also be paralysis. [12]
M.E. may or may not be the same as CFS (Chronic Fatigue Syndrome). This is because there are currently 25 case definitions of ME/CFS, some of which are used to diagnose.[13] Of these criteria some have a psychiatric bias; others have a more immunological specification.
If the CFS criteria used involves damage to the Central Nervous System, then it could well be the same disease as M.E. Other CFS criteria used, especially the Oxford criteria, focus on patients whose fatigue could be of psychiatric origin and this is not M.E.
The name M.E. has a long medical history of being a neurological disease (see our document ‘Saying No Can Be Positive’ for further medical history to the name), being classified in neurological textbooks since the 1960s.
The name CFS was created in the 1980s with almost exclusive emphasis on the word ‘fatigue’, leaving out much pathology (structural evidence of disease) and previous physical M.E. research findings. The vagueness of the term CFS is thus attractive to insurance companies, drug companies promoting anti-depressants for fatigue and government departments intent on saving money through benefits, support and research programmes. Any illness which has guidelines excluding pathology tends to not be taken seriously by medical authorities and the like.
Therefore, the term CFS can be harmful as a label to M.E. sufferers because it can exclude pathology. Sometimes, however, researchers and medical staff use the term CFS to mean M.E. So the situation is unacceptably confusing. M.E. is a more specific name implying the pathology which has been found.[14] [15]
[1] Clinical Observations of Central Nervous System Dysfunction in Post-Infectious, Acute Onset M.E./CFS from the book The Clinical and Scientific Basis of Myalgic Encephalomyelitis/Chronic Fatigue Syndrome 1992, by Byron Marshall Hyde M.D. The Nightingale Research Foundation ISBN 0-9695662-0-4
[2] What is M.E? What is CFS? Information For Clinicians and lawyers December 2001 E.P.Marshall, M.Williams,
M.Hooper, page 5, available from What is ME (margaretwilliams.me)
[3] Myalgic Encephalomyelitis/Chronic Fatigue Syndrome. A Clinical case Definition and Guidelines for Medical Practioners. An Overview of the Canadian Consensus Document. By Bruce M. Carruthers and Marjorie I. van de Sande, 2005, page 2, published by Carruthers and van de Sande ISBN: 0-9739335-0-X
[4] The Nightingale, Myalgic Encephalomyelitis (M.E.) Definition, 2007 Testable and Non-testable Criteria, pps 7,8 by Byron Marshall Hyde MD, available from www.nightingale.ca
[5] See footnote 4 above (Carruthers) page 1
[6] Ibid
[7] The M.E. Society of America at
https://web.archive.org/web/20130912015313/http://www.cfids-cab.org/MESA/framework.html
[8] See Footnote 4 above (Carruthers) page 1
[9] Dr. Elizabeth Dowsett, The Late Effects of M.E., page 9, The Quarterly Magazine, Summer 2001, The 25% M.E. Group www.25megroup.org
[10] Quote from Dr. John Richardson MB BS, author of book Enteroviral and Toxin mediated Myalgic Encephalomyelitis/Chronic Fatigue Syndrome and other Organ Pathologies The Haworth Medical Press, 2001
[11] See footnote 10
[12] The M.E. symptom list – The Hummingbirds’ Foundation for M.E. (hfme.org) under muscular signs and symptoms
[13] https://translational-medicine.biomedcentral.com/articles/10.1186/s12967-020-02455-0
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3918975/
[14] Pathology of the Central Nervous System and Immune System has been demonstrated. Editorial, Anthony Komaroff, Professor of Medicine, Harvard Medical School, JAMA 2000:108:2:169-171
[15] Vascular dysfunctions in M.E. have been pathologically demonstrated. See the ‘Report’ in the introduction section, The Nightingale, Myalgic Encephalomyelitis (M.E.) Definition by Dr. Byron Hyde. The Nightingale Research Foundation, Ottawa, Canada www.nightingale.ca
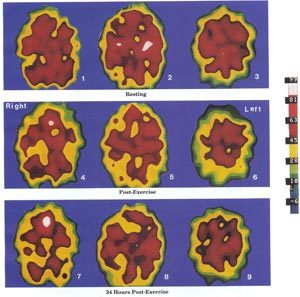
Xenon SPECT scansThese Xenon SPECT scans show pathological brain changes in a 37 year-old female M.E. patient. They show abnormally decreased brain perfusion (blood flow) which decreases further after exercise. In contrast, a healthy person’s brain would normally show an increase in brain perfusion (blood flow) after exercise. Dr. Byron Hyde from the Nightingale Research Foundation, Canada, believes that every M.E. patient has some kind of abnormal SPECT scan. (Reference page 7, The Nightingale, Myalgic Encephalomyelitis M.E. Definition, 2007 :- The SPECT scans (right) are provided by Dr. Jay Goldstein. (Reference page vii of the book, The Clinical and Scientific Basis of Myalgic Encephalomyelitis Chronic Fatigue Syndrome published by The Nightingale Research Foundation 1992) |